Endoscopic tympanoplasty is done for perforated tympanic membrane by stitchless endoscopic technique.
Endoscopic Endonasal Excision of Clval Chordoma by By Dr Khageswar Rout, Asso Prof, ENT, KIMS
Skull base is portion of skull that forms the bottom of the Brain and the bony ridge behind the nose and eyes. Skull base tumors are not a particular type of brain tumor but those that grow in a particular location of skull. Signs and symptoms of skull base tumors depend on the type, location and size of the tumor.
- Most skull base tumors grow inside of the skull, but some form on the outside. Tumors may originate in the skull base or spread there from cancer elsewhere in the body (metastatic).
- Treating skull base tumors and conditions is challenging because they are close to critical nerves and blood vessels in the brain, head, neck, and spinal cord
- Skull base tumors can sometimes be removed surgically. Techniques include minimally invasive endonasal endoscopic removal through the nose or through a small incision in the eyebrow or behind the ear.
- There is no obvious cause for skull base tumors. Radiation therapy to the head, specific genetic conditions and exposure to certain toxic chemicals may increase the risk.
Chordoma are locally invasive slow growing malignant tumors that arise from the remnant of the primitive notochord. The evidence for this is the location of the tumors (along the neuraxis), the similar immunohistochemical staining patterns, and the demonstration that notochordal cells are preferentially left behind in the clivus and sacrococcygeal regions when the remainder of the notochord regresses during fetal life. Incidence rate of chordoma is 0.08 to 0.09 per 100,000. Approximately 40% of chordomas and chondrosarcomas arise in the clivus (directly below the sella turcica and pituitary gland). Chordomas can behave quite aggressively and are often extensively invasive into surrounding skull base structures. A small subset of patients (-10%) may develop metastases to distant sites beyond their site of origin.
Clival chordomas become symptomatic by slow growth and local invasion of adjacent cranial nerves, typically abducens (CN VI), and brainstern structures. These tumors have been treated with extensive resections, with or without radiotherapy. Due to their location in the ventral midline skull base, the transnasal endoscopic approach to the clivus is gold standard as it avoids cerebral retraction, reduces the incidence of injury to the lower cranial nerves, avoids external scars, is relatively quick, helps preserve the anatomical structures and appears to have good surgical outcomes.
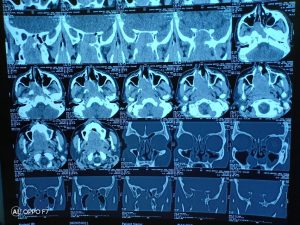
These skull base tumors are best diagnosed by MRI and CT scans which will clearly show the extent of tumor and bony destruction. Focused MR’s of the pituitary region, sinuses, temporal bones or internal auditory canals may be indicated to obtain better anatomical detail of a chordoma.
Other tests may also be needed prior to surgery such as angiography (typically now performed as a CT angiogram or an MR angiogram), visual field tests, an audiogram or pituitary hormonal tests.
Chordomas are relatively radioresistant, requiring high doses of radiation to be controlled. The proximity of chordomas to vital neurological structures such as the brain stem and nerves limits the dose of radiation that can safely be delivered. Therefore, highly focused radiation such as proton therapy and carbon ion therapy are more effective than conventional x-ray radiation. Occasionally, these tumors require multiple keyhole operations including the retrosigmoid and eyebrow craniotomy approaches.
The most common presenting symptom of a clival chordoma is double vision. Less common symptoms may include visual loss, hearing loss, difficulty swallowing, facial numbness, incoordination and motor weakness and nasal congestion.
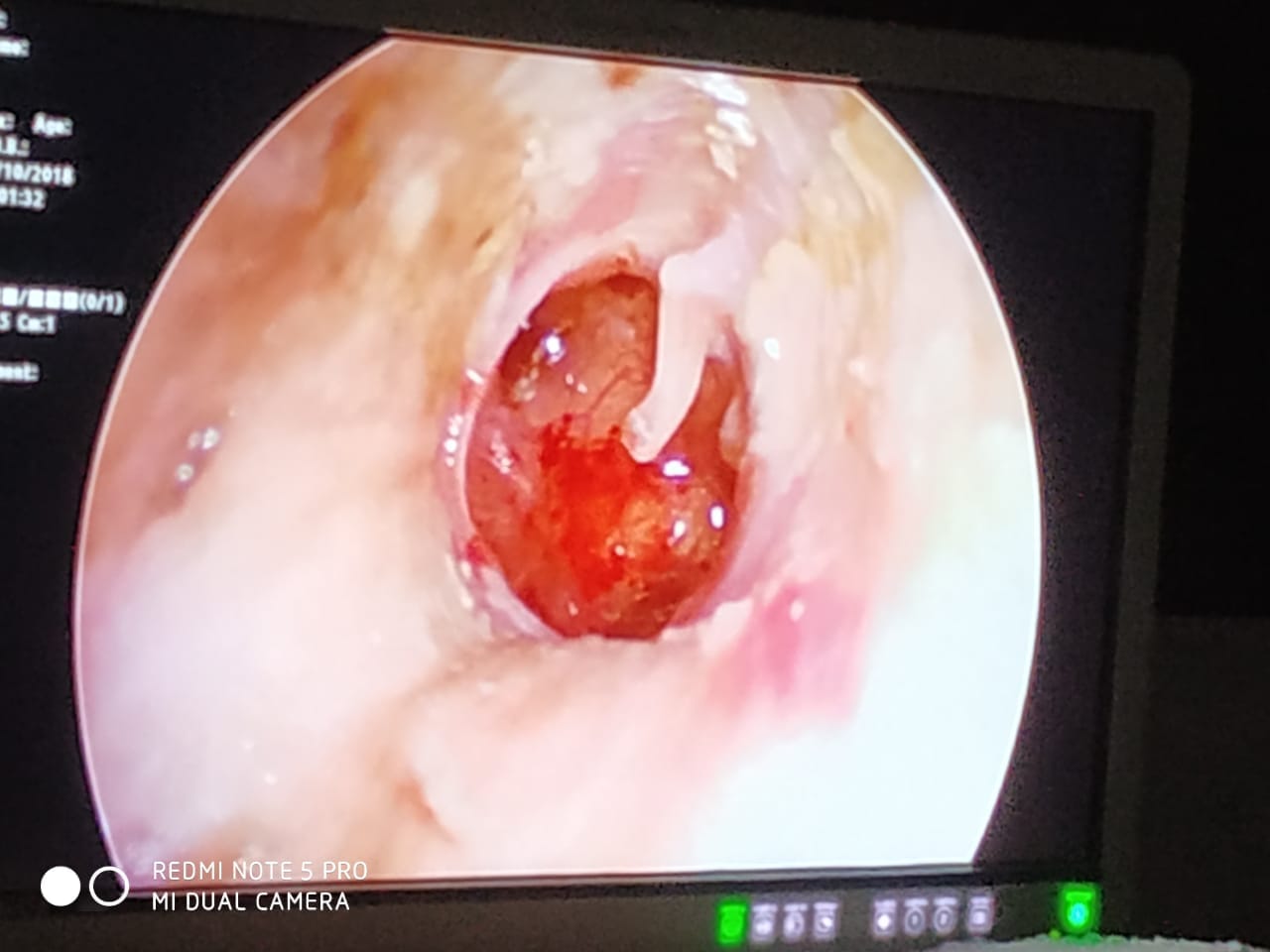
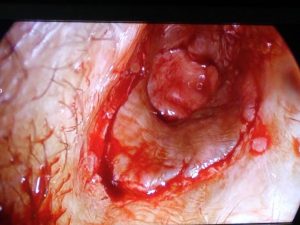
We have treated a very rare case of skull base tumor in the Department of ENT, KIMS. Patient was 68 years male complaining of dysphagia, bilateral nasal obstruction and diplopia since last two years. Biopy done elsewhere came out as inconclusive diagnosis. We did a diagnostic endoscopy and found that, tumor was originating from skullbase.
MRI angiography showed well defined mass filling whole of sphenoid sinus, extending to clivus, extending till anterior portion of C3 cervical vertebra and there was significant extension to left side Parapharyngeal space. Patient was taken for surgery with high risk consent as he was having old AMI. By Endoscopic endonasal approach, posterior septectomy done, sphenoidectomy done, entire tumor with its extension was dissected out in ENT OT in presence of Nurosrgeons.
Surgery was carried out by Dr. Khageswar Rout, Asso. Prof, Prof. R. N. Biswal, Dr. N. K. Das (neurosurgeon), in presence of Anaesthesist, Prof. A. Pradhan and Dr. Saswati Das which took around four hours. Tumor tissue sent for histopathology study came out as Chordoma. Post operative period was uneventful and patient got relief of symptoms immediately and shifted to ENT ward same day.
Skull base chordomas have a notorious tendency to recur even after wide radical removal of the soft tissue and osseous tumor and extensive drilling removal of surrounding bone. Their high recurrence rates warrant adjuvant high-dose radiation therapy.
This combination of radical removal and high-dose radiotherapy delays the time of recurrence, but in most cases, the tumor eventually recurs locally. Clival chordomas are ideally treated with maximal safe surgical removal followed by focused radiotherapy. Fortunately, the majority of clival chordomas can be removed via the nose using an endonasal endoscopic approach.
Initial treatment for a clival chordoma is with surgical removal or debulking. Given their midline location, most clival chordomas and chondrosarcomas are best removed via an endonasal endoscopic approach. However, some extensive and/or laterally placed chordomas may require different skull base surgical approaches. Because chordomas typically invade the bone and dura of the skull base as well as cavernous sinus area, complete surgical resection is often not possible and continued growth of residual tumor is common. Extensive surgery can certainly improve long term survival but over aggressive tumor removal can be associated with significant neurological complications.
Conclusion
EEEA is a safe, well-tolerated and effective surgical treatment modality in the management of ventral skull base lesions. It should be performed with close interdisciplinary collaboration. Appropriate case selection is mandatory. However, despite improved reconstruction techniques, postoperative CSF leakage still remains a challenge.
The endoscopic endonasal approach has become the preferred surgical approach to many tumors of ventral skull base, both benign and malignant. This approach represents an amalgamation of various surgical techniques that have allowed the concepts of minimally invasive surgery to be applied to ventral skull base surgery. Radiologists play an important role in the multidisciplinary skull base team and provide information for surgical planning, post operative management and follow-up.